One year after the United Kingdom legalized medical marijuana, health officials have approved two cannabis-based medicines designed to help treat multiple sclerosis and rare forms of epilepsy.
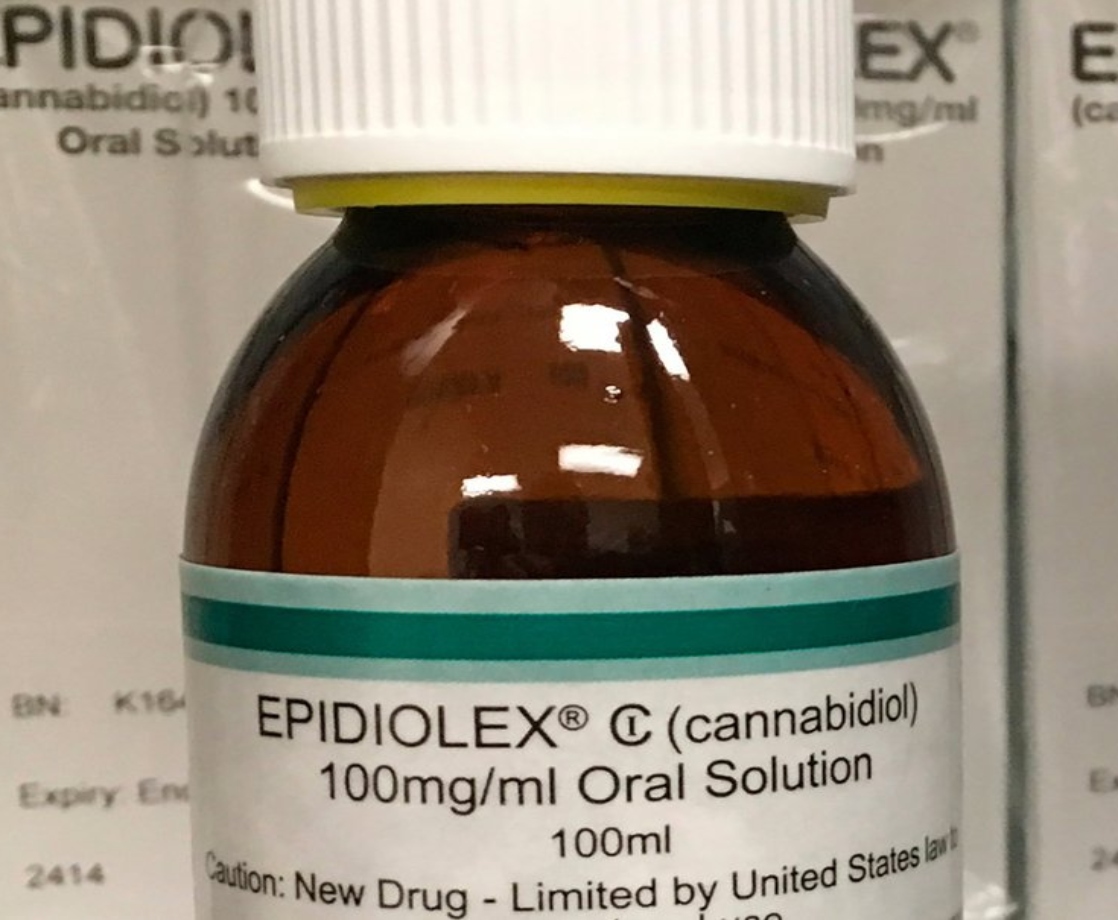
This week, the National Institute for Health and Care Excellence (NICE) approved Epidyolex, a CBD-based oral solution, to treat Lennox-Gastaut syndrome and Dravet syndrome, two rare forms of epilepsy. In clinical trials, this medicine has been shown to reduce the number of seizures by up to 40 percent. This medicine was approved in the US last year, becoming the country’s first legal cannabis-derived medicine, and was approved for use in Europe this September.
A second drug, Sativex, which uses a blend of THC and CBD to treat moderate to severe spasticity in adult multiple sclerosis patients, was also approved. But although this drug is effective at treating symptoms of chronic pain, NICE officially forbids doctors from prescribing THC-based medicines to treat pain symptoms. These two new drugs will soon be available via the National Health Service (NHS), Britain’s government-operated healthcare system.
Sativex was already approved for use in Wales in 2014, but regulators in England ruled that the drug’s price of £2,000 per year per patient was not cost effective. Regulators reversed that decision this week, which will allow doctors in England and Northern Ireland to prescribe this drug. Epidyolex was also initially rejected over its high cost, which comes in at between £5,000 and £10,000 per patient per year. The NHS reached a deal with GW to provide the drug for a lower price, however.
“News that NICE is recommending the use of pharmaceutical-grade CBD (Epidyolex) in the treatment of those with Dravet or Lennox Gastaut syndromes will bring hope to many families affected by these two severe forms of epilepsy,” said Professor Ley Sander, medical director at the Epilepsy Society, according to Pulse Today. “The need for new treatment options is unquestionable and it is reassuring that the new medication has been through clinical trials and regulatory processes.”
While some have applauded the UK for finally making these medications legal, others are outraged that the government’s approach to medical cannabis reform has been so slow. Millie Hinton of advocacy group End Our Pain told The Guardian that these new approvals were “a massive missed opportunity” to legalize a wider range of cannabis-based medicines.
“It is particularly devastating that there is no positive recommendation that the NHS should allow prescribing of whole-plant medical cannabis containing both CBD and THC in appropriate cases of intractable childhood epilepsy,” Hinton said. “It is this kind of whole plant extract that has been shown to be life-transforming for a significant number of children.”
The UK Home Office officially began allowing specialist doctors to prescribe medical marijuana last November. Most doctors have been unwilling to write these prescriptions, however, citing a lack of clinical evidence proving that medical cannabis can effectively treat these conditions. This situation has forced parents of epilpetic children to import expensive medical cannabis products at their own cost.
“Though this is disappointing, we appreciate that clinical research is vital to ensure that any treatment recommended for use in the NHS is safe and effective,” said Simon Wigglesworth, deputy chief executive at Epilepsy Action, to The Guardian. “We are aware of ongoing efforts to bring forward research into cannabis-based medicines for epilepsy, including those containing THC, at pace.”