Taeia Kaley-Dolan was sick for two years before she realized she had cannabis hyperemesis syndrome.
In 2014, she began smoking weed for anxiety and depression following the death of her brother. Soon, she started retching up mucous and feeling intense abdominal pain. “I could feel my heartbeat in my stomach,” Kaley-Dolan describes. “I blamed it on stress. I basically continued to smoke to take more of the edge off.” But it got worse. The daily nausea began to kick in, then the vomiting. It felt like a flu that wouldn’t go away.
“I went all day puking, wondering what I could do to stop it,” she says. The now 19-year-old Ohioan realized hot baths or showers, plus weed, made her feel better, especially given cannabis’ capacity for suppressing nausea.
Unfortunately, the relief that weed and warm water brought her didn’t last. Kaley-Dolan started smoking more, and getting sick at least twice as often. She went to the hospital for tests that left both her and doctors clueless. She lost jobs and friends, missed school, and couldn’t leave the house for more than a couple hours without having to bolt to a bathroom. She went from smoking a gram or two per week, to about half an ounce; cannabis was the only thing that relieved her symptoms. Unbeknownst to her, it was also the reason she was sick.
“I stand by the medical properties of cannabis so much; I respect what it’s done for so many people, so I didn’t know what I was doing wrong,” she says. “Finally I came across [an] article about cannabinoid hyperemesis syndrome.” It described her symptoms to a T.
Related: Here’s What Bad Weed Looks Like
In recent months, cannabis hyperemesis syndrome has picked up more media attention, especially around the turn of the year. (Kaley-Dolan, however, found out about it in April 2017.) As a purported phenomenon unfolding in states with newly legal cannabis, such as Colorado and Washington, it’s still unclear how prevalent the syndrome actually is. With sensational headlines in international publications calling it a “mysterious” and “bizarre” vomiting condition that compels victims to take hot baths and visit the emergency room, little is known about cannabis hyperemesis syndrome beyond its connection to weed. More nuanced takes on the syndrome are rare, but they point to other factors like specific strain qualities, molds and pesticides, or particular terpenes.
Source: CBSNews.com
There were no documented cases of cannabis (or cannabinoid) hyperemesis syndrome before 2004. “I started to dig into it, and my boyfriend and I found a bunch of these articles about azadirachtin poisoning,” says Kaley-Dolan.
Azadirachtin is an organic pesticide extracted from neem oil. It’s approved by the Organic Materials Review Institute (OMRI), which means it’s vastly safer to use than nastier, inorganic pesticides like myclobutanil. Considered the lesser of many evils, it became popular with conscientious cannabis farmers in the early aughts — around 2004.
“More so recently you see a lot of these people with this syndrome and they’re stuck thinking it’s the cannabis, but it’s not; it’s the azadirachtin poisoning,” says Kaley-Dolan. “It builds up in your system over time and that’s what’s toxic, and your body rejects it by throwing it up. The reason the cannabis works so well is that it’s antiemetic; it makes you not nauseous. You feel better, but over time, the azadirachtin levels in your body overpower all the antiemetic properties of cannabis. That’s what happened to me. I smoked until I couldn’t smoke any more.”
In May, Kaley-Dolan tried going to prom. She got all dressed up in an effort to enjoy the last bit of high school, but regrettably she got sick again and was finally hospitalized. Completely dehydrated from vomiting, she admitted to the hospital staff in Auburn, Ohio — where a limited medical marijuana law applies only to those with qualifying conditions — that she’d been smoking black market weed. She’s since been off cannabis, and on a number of pharmaceuticals to treat not just her remaining nausea, but also tangential conditions she’d developed on account of unintentionally poisoning herself for two years.
To get the word out about the distinction between cannabis hyperemesis syndrome and azadirachtin poisoning, Kaley-Dolan’s boyfriend Maxwell Phillips sent a link to Instagram celebrity Tony Greenhand, who’s famous for making “smokeable art” out of joints and blunts. Greenhand reposted it, garnering hundreds of likes and comments.
“Cannabis hyperemesis is not a thing,” Greenhand wrote in an email to MERRY JANE. “What we think is cannabis hyperemesis IS [actually] azadirachtin poisoning. Cannabis hyperemesis was invented due to the symptoms created from azadirachtin poisoning.”
Neem oil, from which azadirachtin is derived, is a common pesticide and fungicide that’s been used in cannabis farming for many years to ward off spider mites, invasive bacteria, and other pests. However, neem oil can be difficult to apply and needs to be kept warm in order to remain a liquid. “If sprayed on cannabis flowers, neem oil does not dissolve or evaporate for long periods of time, directly affecting the naturally occurring oils and terpenes,” explains Greenhand, a former cannabis grower. “In its concentrated form, azadirachtin does not solidify at room temperature and is easier to apply.”
Azadirachtin products like Azatrol, Azamax, and Azasol are supposed to stay on the plant residually for about 21 days. Typically, they shouldn’t be sprayed after the fourth week of the grow cycle, but some growers spray later if they have an infestation. That means the chemicals might still be on the plant by the time it gets to the consumer.
“I’ve never met a grower who, at the very least, doesn’t use neem oil,” says Brandon Neff, a medical marijuana farmer from Oregon. “A lot of other people in my area use Azamax and other products. It’s something no grower really wants to have to use, but when I try to go and use the beneficial bug route [using insects to deter more destructive pests], sometimes the mites are more resilient. It’s a bad issue: You don’t want to harm the plant, but no grower wants to be responsible for additional harm to the patient. We only want to help heal.”
Neem itself is a highly medicinal plant, used for centuries in India’s ayurveda medicinal practice and as a part of integrative healthcare. Health food stores even sell neem toothpaste. Azadirachtin, one of the active ingredients in neem, serves as an insect growth regulator, preventing pests from reproducing when it’s sprayed on plants.
“A lot of organic farmers who are well intentioned are using these pesticides because they’re on approved lists of what can be used and are OMRI certified,” says Alec Dixon, co-founder of SC Laboratories in California. “The most important thing to recognize is the way people are using these pesticides. Even organic pesticides can be applied improperly.” At face value, azadirachtin might be no more harmful than other types of horticultural oils like rosemary or peppermint, he adds, but growers still need to use them cautiously. “If they’re using these products late into the flowering cycle, a few weeks leading up to harvest, there’s a guarantee that you’re leaving residue behind on the flower.”
And the build up of that residual azadirachtin in heavy smokers might cause cannabis hyperemesis syndrome — but we don’t know for sure. Correlation doesn’t necessarily mean causation, Dixon points out.
In 2013, an acute case of neem oil toxicity was documented in the Indian Journal of Critical Care Medicine. Among other symptoms, the patient suffered from nausea and vomiting. Other cases of poisoning have since been reported in India, where neem is widely used.
Traditionally, neem has been used to treat a variety of health conditions including inflammation, colds, flu, gum disease, heart disease, high blood pressure, pain, athlete’s foot, and scabies among others. However, for the small number of people who are allergic or sensitive to neem, it doesn’t come without side effects, such as abnormal heart rhythms, low blood pressure, anemia, cardiac arrest, loose stools, liver damage, seizures, or vomiting. These go above and beyond the basic symptoms of cannabis hyperemesis syndrome.
Azidiractha Indica, more commonly known as a neem tree. Source: Wikimedia Commons
Some argue that azadirachtin poisoning and cannabis hyperemesis are completely different phenomena.
“It doesn’t make any physiological sense that those two would be linked together,” says Dr. Jeffrey Raber, founder of the Werc Shop, a lab testing facility in Los Angeles. “You’d be able to see the same syndrome without the cannabinoids.” Raber describes cannabis hyperemesis syndrome as an overactivation of the body’s endocannabinoid system. “It’s saying, ‘Get this out of me’,” he says. “We’ve been able to see people who had the syndrome mitigated through the reintroduction of terpenes and fewer cannabinoids.”
Moreover, azadirachtin was introduced to the market well before cannabis hyperemesis syndrome was first documented. The EPA first registered azadirachtin for use on food crops in 1990, according to Murray Isman, University of British Columbia professor of entomology and toxicology, with a specialty in natural pesticide botanicals. For decades now, it’s been used extensively on food crops throughout North America, Europe, the Caribbean, and Sub-Saharan Africa. The California Department of Pesticide Registration, for instance, published that nearly 4,000 pounds of azadirachtin were applied to crops in 2014, including 1,000 pounds on strawberries and 440 pounds on lettuce.
“It’s probably one of the safest pest control products on the market place,” says Isman. “I have never heard of a single case of azadirachtin poisoning in a human in the U.S.” Azadirachtin itself is a triterpene chemical, Isman explains, meaning that it wouldn’t be an allergen anyways, since all allergens are proteins and peptides.
“Having said that, Azamax is 1.2 percent azadirachtin, which means the rest of the formula is solvents and all the other stuff that makes a pesticide a pesticide,” Isman adds. “That’s not to say there isn’t something in all the other stuff that couldn’t cause a GI reaction, but it’s really unlikely. It’s used on food crops all the time.”
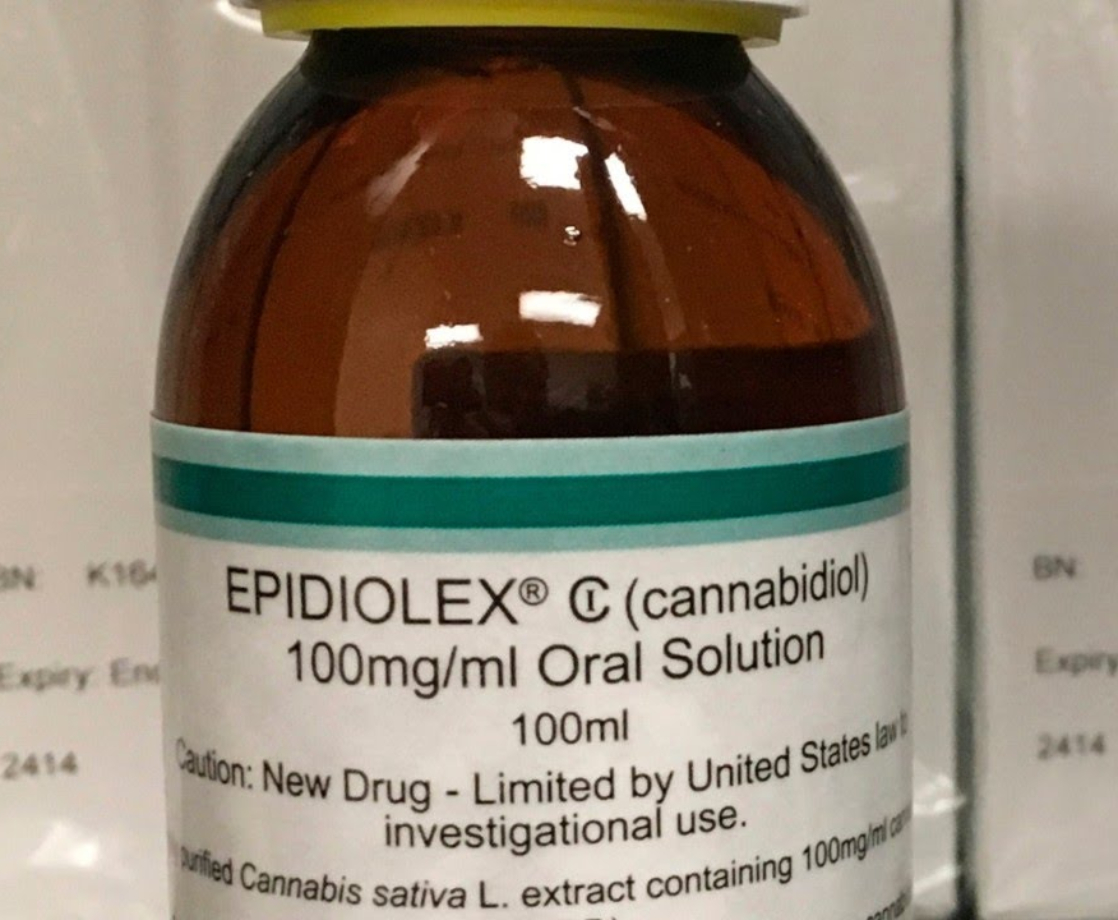
Karl Young, director of Hermetic Botanicals, a company that makes remedies for cannabis hyperemesis syndrome, also says there’s no direct link to azadirachtin poisoning. He suggests that the only way way azadirachtin might potentiate cannabis hyperemesis syndrome is if it causes gallbladder dysfunction. In such cases, an imbalance of the body’s enzymes would make it such that the body gets overloaded with CBD.
CBD plays a distinct role in cannabis hyperemesis syndrome. “In animals, the effect of CBD on toxin-induced vomiting displays a biphasic response, with low doses producing an anti-emetic effect, whereas higher doses enhance vomiting,” according to a 2011 study published in Curr Drug Abuse Review.
Whatever role, if any, that azadirachtin plays in cannabis hyperemesis syndrome, there’s a risk in trying to eliminate the use of this organic pesticide altogether. Since such a tiny percentage of cannabis consumers are affected by the syndrome, it may not make sense or be likely for the industry to change its cultivation practices en masse. “A lot of people would be dealing with huge potential catastrophic losses of bug infestation or mold powdery mildew on crop,” says Dixon. “The worst thing that can happen because of this loose correlation is all of a sudden organic pesticides get cracked down on as much as nonorganic pesticides, and it ties the farmers’ hands; they can’t spray anything organic. That opens it up to GMO cropping.” A company like Monsanto could hypothetically come in with genetically modified plants that are inherently resistant to pests and outcompete small farmers lacking the same resources, Dixon fears.
Instead of relying only on azadirachtin, outdoor Mendocino farmer Justin Calvino (a board member of the California Growers Association) suggests diversifying pest management strategies. Instead of using neem oil or a derivative, farmers can use good insects to kill the bad ones. To defend against pests, Calvino suggests not only a clean environment and castor oil soaps, but also other plant-based nutrients like grape seed oil or olive oil. Even so, he admits, “if you’re concentrating it to the level you’re seeing it being concentrated, people are getting sick.”
So while there may be no conclusive answer for the cannabis industry and consumers alike regarding what biological dynamics cause cannabis hyperemesis syndrome yet, what arguably holds back deeper medical research is the plant’s prohibited status under federal law. Until marijuana can be scientifically studied without onerous legal roadblocks, health issues like this will be continually debated by users, cultivators, and regulators in canna-legal states.
As for Kaley-Dolan, she says once she’s completely healed from her cannabis hyperemesis syndrome, she wants to grow her own weed. “I still have a hard time eating, and I still take a lot of baths, but I haven’t been sick in about [two months] now and I’m continuing to make a lot of progress,” she says. “I had no idea I was chasing my tail for literally two years. Once it’s legal to grow my own, I should just do that so I know 100 percent what’s in it. I just want to feel safe on that side of things.”
Illustrations by Nick Humbel